Do you get enough deep, restorative sleep?
I’ve been helping my patients to sleep better for many years. I’d estimate that 70% of everyone I’ve asked says their sleep isn’t optimal. And perhaps 35-40% say it’s really a problem. And an unknown additional percent have a sleep disorder, but aren’t aware of it. In our always-on, brightly lit culture, good sleep is a vanishing commodity.
 (http://quantdoctor NULL.com/wp-content/uploads/2011/06/zeo1 NULL.png)
(http://quantdoctor NULL.com/wp-content/uploads/2011/06/zeo1 NULL.png)A Sleep Hacker Wearing the Zeo Headband
Typically there really was no telling what was actually going on for a patient at night. Except for a few where I could get polysomnography (http://en NULL.wikipedia NULL.org/wiki/Polysomnography) done in a sleep lab – a procedure too costly and unavailable for most people.
For obstructive sleep apnea, I sometimes would use rough measures like an audio tape recorder at the bedside, or reliable reporting from a spouse, to detect loud snoring or audible apneas. But sleep apnea is only one of many possible sleep problems, and can be inaudible.
For most, it was hard to know whether their self-reported sleep duration was accurate, or whether the hours they were spending in bed were good quality sleep, or fragmented and disrupted sleep. Environment, diet, alcohol, stress, mood, medical conditions, and many other factors can impact sleep. Add in prescription medication effects (from beta blockers to antihistamines, many medications disrupt deep and REM sleep), and it can become a challengingly complex situation to figure out.
I’ve recommended various strategies to experiment with the sleep environment, sleep behaviors, mind-body techniques, diet, supplements, and medications, and to implement various other strategies to improve sleep quality and quantity. And often with a fair amount of success.
But now we are starting to get some affordable tools that will tighten the feedback loop and provide real measures of success as we try to improve sleep. One such sensor device is the Zeo (http://myzeo NULL.com/).
 (http://quantdoctor NULL.com/wp-content/uploads/2011/06/zeo_jun91 NULL.png)
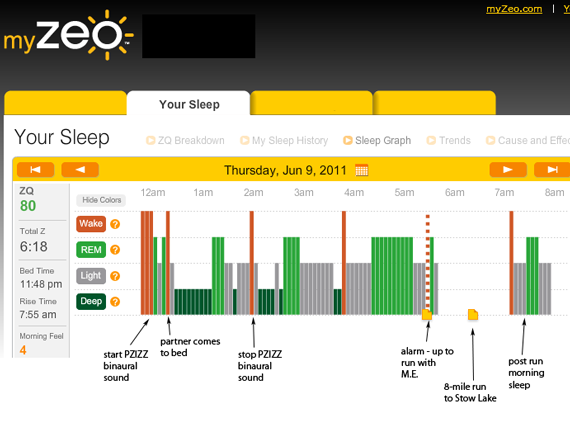
(http://quantdoctor NULL.com/wp-content/uploads/2011/06/zeo_jun91 NULL.png)Dr. Abramson's Zeo data from 6/9/11
The Zeo is a 3-electrode EEG sensor attached to the forehead with a soft headband. A medical-grade EEG setup it’s not, and it is officially a non-FDA-approved, non-medical consumer device. Nonetheless it seems to be able to get a reasonably accurate estimate of sleep stage in 30-second intervals throughout the night in the several people I have tested it on, and at $200 it’s an order of magnitude more affordable than a typical overnight polysomnogram study. [Ed.: the above paragraph was corrected based on comments received]
By correlating the Zeo data with my own memory of the night’s events, it’s possibly to get a better idea of what’s going on. Does my partner entering bed at 12:20am disrupt my sleep significantly? Apparently not – I entered deep sleep shortly therafter for almost an hour. Does the PZIZZ (http://itunes NULL.apple NULL.com/us/app/pzizz-sleep/id341324632?mt=8) binaural sound program help? My jury’s still out – but I can now compare similar nights with and without it, and answer that question. Am I getting enough deep and REM sleep? The night above seems to indicate “yes.” But although I felt pretty good at 8am, I question whether 6:18 is enough total sleep time – we’ll see.
 (http://quantdoctor NULL.com/wp-content/uploads/2011/06/bedside1 NULL.png)
(http://quantdoctor NULL.com/wp-content/uploads/2011/06/bedside1 NULL.png)- The Quant Doctor’s Nightstand
Of course, many people will be able to use the Zeo independently to improve their own sleep, without involving a doctor. But if they happen to be working with a doctor on almost any health problem (from chronic fatigue, to heart disease, to alcoholism, to rheumatoid arthritis), having data on sleep can be an invaluable piece of the puzzle. [ I co-wrote the chapter on “Sleep and Inflammation” in the Oxford University Press book Integrative Rheumatology (http://www NULL.amazon NULL.com/Integrative-Rheumatology-Weil-Medicine-Library/dp/0195311213/ref=sr_1_1?s=books&ie=UTF8&qid=1307912869&sr=1-1) (part of the Weil Integrative Medicine Library), detailing how sleep and inflammatory conditions are tightly linked. ] Or if a patient has particularly challenging sleep issues, a physician can work with them much more productively with this data, and perhaps determine what additional testing and treatment strategies might be the best next step.
The conventional medical world still doesn’t have a lot of sophistication about how sleep can interact with health, and what to do with potentially ubiquitous sleep data being available on everyone. At My Doctor Medical Group (http://mydoctorsf NULL.com) in San Francisco, I am working to develop a model of medicine where doctor and patient work collaboratively to achieve the patient’s goals, where the journey is as important as the destination.
I’ll post more as I gather more Zeo data and correlate it with other data streams.


Hi Dr. Abrahamson. Thank you for writing this article. It is very good. I am interested to see what you have to say about sleep and inflammation.
One correction though: the Zeo uses three electrodes, not two, and the signal quality is actually quite good. In fact, if you strap it around your chest instead of your head and use the serial port on the back with the raw data library you can get a quite clean looking EKG signal. It also measures impedance between the electrodes and generates a “Signal Quality” index based on how good the contact is with the skin, which is also quite useful.
Thanks for the correction about the electrodes, Anne. I will make the correction in my article soon… Sleep and inflammation is a great topic; will write more about it soon.